India’s Healthcare at a Breaking Point: Budget 2026–27 Faces a Make-or-Break Moment
India’s healthcare system reaches a critical crossroads ahead of Budget 2026–27, with experts calling for smarter spending, NCD-focused reforms, digital health integration, and a push beyond 2.5% of GDP in public health investment.

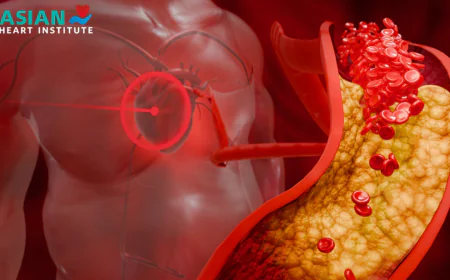
The healthcare sector in India is at a junction before the Union Budget 2026-27, and policymakers, leaders, and industry experts in the sector are pushing it to take a major step in replacing the need to spend more by smart spending. With the rising strain of non-communicable diseases, now constituting approximately 65% of all mortality, the discussion has shifted to the size of the budget to the design, implementation and system resilience in the long term. There are demands among the stakeholders to have a multi-year healthcare road map that enhances primary and preventive care, implants routine screening of the chronic diseases and lessens household out of pocket costs. As the public health expenditure continues to linger at approximately 2% of GDP, some are now placing pressure to exceed the 2.5% mark and support it with structural reforms. The Budget will also see digital health leave pilot projects behind and move to interoperable national platforms, domestic pharma and medical device manufacturers will receive support by addressing tax distortions and urgent gaps in hospital capacity and protection of the healthcare workforce. Budget 2026-27 is not simply a financial exercise to many people but a make-or-buy moment to re-engineer the healthcare future of India.
Why Health Spending Stayed Below 2.5% of GDP Despite Big Promises
India is one example of a country that has been stuck between promise and practice in the last decade by failing to meet its pledge of increasing its spending on public health to 2.5% of GDP. Fiscal priorities competing such as defence, infrastructure, and welfare schemes that have more immediate political optics have continuously crowded out long-term health investment. The low level of tax-to-GDP ratio further constrained the fiscal space, and the health as a state subject, led to the lack of equality in the expenditures and the poor coordination among states. In cases where funds were given out, it failed in implementation because of staff shortage, lack of infrastructure, and slow implementation. The preeminence of a relatively unregulated sector of private healthcare only intensified reliance on out-of-pocket spending, making there less of a sense of urgency to expand the sector publicly. Most importantly, politics did not become an issue of electing relying on healthcare, which curbed political responsibility. Such policies as the National Health Policy 2017 established goals but did not have deadlines or enforcement measures, which could stop but not eliminate the gap each year.

What Budget 2026–27 Is Poised to Change
The Union Budget 2026-27 is emerging as a breakout of incrementalism. In contrast to the careful growth of 2025-26, the new budget should be based on system design, results, and resilience in the long term. The management of non-communicable diseases will be brought to center with increased screening and integration of primary-care. The digital health will likely become interoperable national platforms instead of pilots. Tier 2 incentives to the private hospitals of the 3 cities, duty adjustments in the medical manufacturing, and outcome-based funding model can rebrand the healthcare financing system - marking the transition between promises and performance.